Inteleos Blog: Case of the Quarter
 Author:
Author:
Falguni Patel (BS,RDMS,RVT,RMSKS)
Falu is an advanced pediatric sonographer at Lurie Children’s Hospital of Chicago for over twenty years. She is credentialed by the American Registry of Diagnostic Medical Sonography in Abdomen, Obstetrical and Gynecological, Neurosonology, Pediatric, Vascular Technology, and Musculoskeletal specialties. She serves on the Contrast, Musculoskeletal and Pediatric Imaging committee.
Clinical Information
Neonatal Intensive Care Unit (NICU) nurse brought a two-day old male full-term infant to the X-ray department for a voiding cystourethrogram with the raised concern for posterial urethral valve. The infant had a prenatal history of bilateral hydronephrosis with an enlarged bladder.
Going Above and Beyond
The radiologist, who was on fluroscopy (fluro) saw the patient’s age and history and approached to ask me if the ultrasound department was available to do contrast enhanced Voiding Urosonography (ceVUS) instead of a Voiding Cystourethrogram (VCUG) to avoid additional exposing the patient to additional radiation. The radiologist asked my availability prior to approaching the patient’s Urologist to change the order.
It was not our department’s designated ceVUS day, but I agreed to drop everything and do the procedure, as I believed ceVUS was the best choice to prevent the patient receiving unnecessary radiation. My radiologist contacted the urologist and explained the benefits of ceVUS verses VCUG and the urologist agreed to do ceVUS. He put in a new exam order for ceVUS but kept VCUG as a pending order in the event we had limitations during the CEVUS exam.
Based on the conversation with the urologist, I took the Ultrasound machine to the Fluro room, communicated with the Fluro tech and the patient’s nurse about performing ceVUS in the Fluro room and set up the room for the ceVUS procedure. I initiated the procedure with the team a nurse, an x-ray tech, two radiologists, a resident and a fellow.
While scanning the patient, who came to us in an incubator, without his parents, I realized the crucial role our dedicated team played to make the procedure happen and ensure the patient was safe and received the best possible care. I felt proud to be part of a wonderful team that simply believes in “All for your one”
Brief Description of the Procedure:
The pre-scan for the renal and bladder anatomy was performed. During the procedure, three cycles of bladder filling and voiding were assessed with ultrasound imaging during the administration of a 0.2% solution of Lumason contrast material in normal saline.
Findings:
Imaging of the bladder, ureters and kidneys were performed under contrast ultrasound. The bladder demonstrated normal size, shape and contour. During contrast instillation we identified an immediate bilateral vesicoureteral reflux into the dilated and tortuous bilateral ureters to the level of the kidneys with moderate to marked dilation of the pelvicalyceal systems. A small amount of intrarenal reflux was documented in the left kidney. Voiding the urethra demonstrated a normal configuration with no abrupt caliber change or filling defect.
Ultrasound Images:
Pre-scan Images of Renal and Bladder US:

Transverse Bladder

Longitudinal right ureter

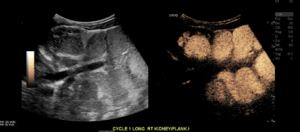
Longitudinal right kidney

Longitudinal left kidney

Longitudinal left kidney

Longitudinal right kidney
Ultrasound Images During Contrast Administration:

Early Filling Longitudinal Bladder
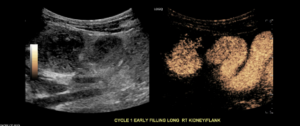
Early Filling Longitudinal Right kidney and Right ureter

Early Filling Longitudinal Left kidney and Left ureter
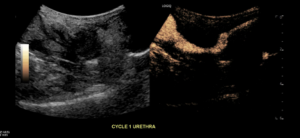
Urethra during voiding phase
Late filling Longitudinal Right and Left Megaureters

Late filling Transverse Right and Left Megaureters
Ultrasound Impression:
Bilateral grade 4-5 vesicoureteral reflux with a small amount of intrarenal reflux demonstrated in the left kidney.
The Importance of Teamwork
Teamwork plays a vital role in our profession. It all comes down to what is best for the patient. This case reminds us not to limit ourselves when it comes to patient care. Instead of simply performing the ordered exam, there are great benefits to being proactive and choosing what is best for the patient. After we performed the ceVUS, our radiologist shared the ultrasound findings with the urologist to see if a VCUG was still required. The results we achieved from the ceVUS procedure proved that the patient had posterior urethral valves and decided to cancel the VCUG exam with appreciation for the team’s work. By working hand in hand with our radiologist – who depends highly on us to provide the best patient care – we prevented a two-day old patient from unnecessary exposure to radiation.